This is my own work and is provided here as an example of how I perform a in-depth image critique but this is not a ‘this is how it must be done’ example.
Clinical history
26-year-old male patient attended the emergency because of pain in his left ankle. The pain had occurred after a backward fall while his left foot stayed fixed to the ground, while playing tennis. The ankle was immediately painful, swollen and the patient was unable to bear weight. He did not have any other complaints or signs of injury.
Image quality
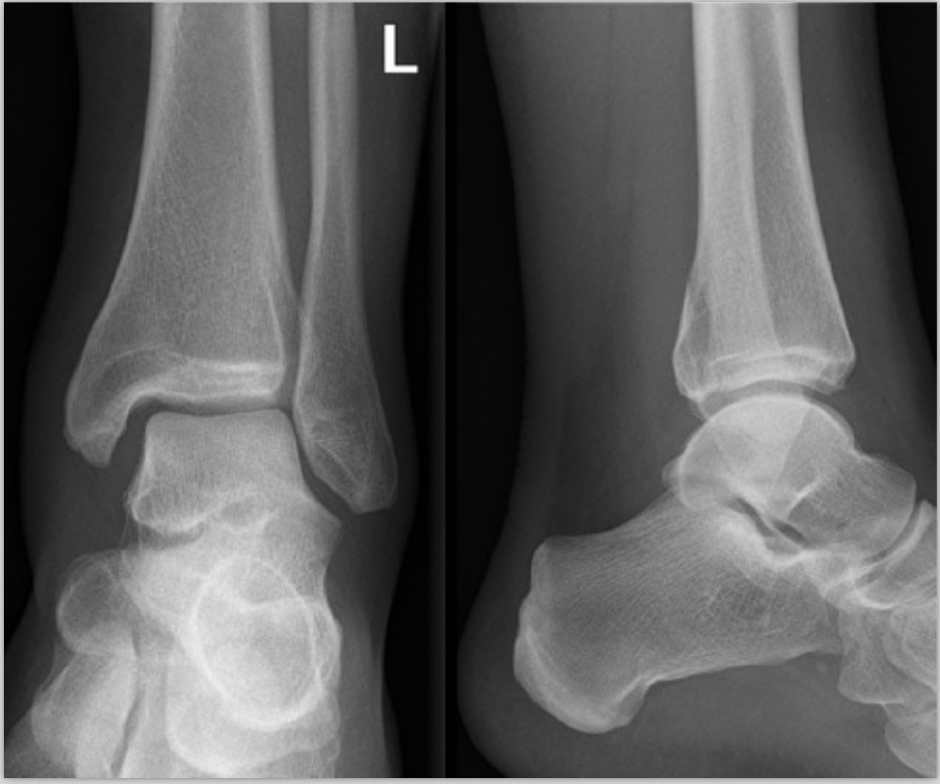
Two view ankle series presented together on a single view. Patient identification has been removed for confidentiality and privacy. A single left post-processed marker is placed on the mortise projection.
The lateral view has appropriate collimation demonstrating the required anatomy from the distal third of the tibia and fibula, to the proximal aspect of the metatarsals (Bell & Gorton, 2018). Although the AP mortise view is similarly collimated, according to Bell and Gorton (2018) the AP mortise view should have included the base of the 5th metatarsal in the inferior aspect of the image. The AP mortise view appropriately includes the skin margins laterally and the lateral view demonstrates soft tissue margins anteroposteriorly.
In terms of patient positioning, the AP mortise view demonstrates both the lateral and medial malleoli in profile. However, there is non-uniformity of the mortise joint suggestive of a pathological process (discussed later). The lateral projection was performed appropriately with the distal fibula projected over the posterior half of the distal tibia. The talar domes are superimposed allowing appropriate visualisation of the superior talar articular surface. The tibia-talar joint is seen in profile.
Without appropriate collimation borders it is not possible to accurately comment on the location of the central x-ray beam (CR) in any of the images but using the visible shuttering borders as a guide, the CR appears to have been directed at the midpoint of the lateral and medial malleoli over the tibia-talar joint on the AP view. On the lateral view, the CR should have been projected over the bony prominence of the medial malleolus of the distal tibia but it has been centred at a point behind the tibia and fibula.
In terms of radiographic density, all radiographs are adequately exposed because the lateral skin margins of the ankle are visible. Further, the lateral view distinctively demonstrate kager’s fat pad suggesting that an appropriate mAs was selected for the examinations. This series demonstrates high radiographic contrast with visualisation of the cortical outlines and trabeculae; suggesting that appropriate kVp were selected to demonstrate the ankle anatomy.
Radiological description of pathology
As mentioned previously, the mortise view demonstrates subtle non-uniformity of the mortise joint as indicated by medial mortise widening, suggestive of syndesmotic instability. There are two cortical breaches on the lateral view – on the posterior surface of the tibia and inferior articular surface of the tibia.
Diagnosis
Note is given to the instability of the distal tibiofibular syndesmosis and fracture of the posterior tibial malleolus following traumatic injury. Although this is atypical presentation, this patient might present with a complex injury similar to a Maisonneuve fracture where there is usually tibiofibular syndesmosis injury, widening of the ankle joint and other associated fractures such as pilon tibiale, lower leg spiral shaft fractures and malleolar ligamentous injury (Bell & Weerakkody, 2018; Smeeing et al., 2017). Given the patient’s clinical history, other traumatic fractures are possible on the ipsilateral long bone. Further clinical correlation is needed and extra views of the lower legs are suggested.
Further imaging
To exclude other traumatic fractures, it would be justified to perform further imaging of the entire tibia/fibula complex for other associated fractures (Smeeing et al., 2017).
A CT examination of the ankle joint should be requested for further investigation of the posterior malleolar fracture and syndesmotic instability (Smeeing et al., 2017). If the extra plain radiograph views are diagnostic for other injuries, it would be justified to perform a CT through that area too.
References
Bell, D., & Gorton, S. (2018). Ankle (mortise view). Retrieved from https://radiopaedia.org/articles/ankle-mortise-view?lang=us
Bell, D., & Weerakkody, Y. (2018). Maisonneuve fracture. Retrieved from https://radiopaedia.org/articles/maisonneuve-fracture
Hacking, C., & Jones, J. (2018). Ankle x-ray (summary). Retrieved from https://radiopaedia.org/articles/ankle-x-ray-summary
Smeeing, D. P. J., Houwert, R. M., Kruyt, M. C., & Hietbrink, F. (2017). The isolated posterior malleolar fracture and syndesmotic instability: A case report and review of the literature. International journal of surgery case reports, 41, 360-365. doi:10.1016/j.ijscr.2017.10.062
0 comments on “Image critique example – ankle series” Add yours →